|
actions to expand pharmacist-provided care 
Healthcare PayersHealthcare payers, including health plans and insurance companies, can consider taking five actions to strengthen partnerships with pharmacists to deliver value-based pharmacist-provided care that improve patient outcomes. The perspectives of the pharmacists and payers participating in an industry survey and multi-stakeholder roundtable are the basis for these recommendations. 
Form risk sharing partnerships with community pharmacies in a sustainable way to deliver patient care.Healthcare payer organizations can partner with community pharmacies in value-based, risk sharing partnerships that reward pharmacists for providing evidence-based clinical care that improves patient health and reduces the burden of chronic disease. When successful, these partnerships can provide models of financially sustainable, pharmacist-provided patient care that can be replicated throughout the healthcare system. Increased payer support of these patient care services will accelerate pharmacists' progressive transformation to value-based care and the ability of pharmacy organizations to meet the needs of patients and payers.
Implement hybrid reimbursement models with pharmacies that combine fee-for-service with value-based care.Sustainable partnerships with payers in the provision of pharmacist-provided care provides pharmacists with the opportunity to diversify and strengthen revenue streams in today’s competitive healthcare market. Building on and separate from dispensing services, a combination of fee-for-service and pay-for-performance arrangements can help pharmacy organizations sustainably transition to a value-based business model. These arrangements have shown promise in some Medicare Part D programs, specialty pharmacies and chronic care management programs.
Establish a system-wide infrastructure to support value-based contracts.A well-designed, system-wide infrastructure for tracking the progress of pharmacists and pharmacy organizations and supporting them in value-based, pay-for-performance agreements with payers exists, but opportunity for its expansion beyond Medicare and into other insurance lines of business including Medicaid and commercial should be pursued. This infrastructure should remain focused on industry-endorsed quality metrics, pharmacist performance goals and patient outcomes and aim to align the needs of pharmacists and payers and foster greater care quality and efficiency. Furthermore, a system-wide model that is secure, transparent and interoperable will support consistent care across patient populations and enable the broader use of value-based contracts. 
Improve data sharing to enhance pharmacists’ role in outcomes-based healthcare.The channels to share data between payers and pharmacists exist, but shared investment and collaboration is required to leverage them and optimize patient care and outcomes. Linking pharmacy data with other clinical care data and payer claims data through improved infrastructure and sharing agreements will position pharmacists to play a greater role in outcomes-based healthcare. Collaborations and joint investments among pharmacists, payers and technology vendors can improve access to and utilization of standardized healthcare data to inform patient care. By integrating pharmacy data with other clinical data, including diagnoses, procedures, screenings and laboratory results, pharmacists can be positioned to provide patient care that is more holistically evaluated for its impact on patient outcomes.

Use outcomes-based quality performance measure sets to align pharmacy services in vertically-integrated clinical care.Vertical integration in healthcare can create efficiencies and provide higher-value care, but its success depends on aligning efforts and quality improvement across the care continuum. The development of outcomes-based performance measures and their use with structural and process measures as part of vertically-integrated measure sets will provide pharmacists opportunities to further demonstrate their value in team-based care, as the clinicians most accessible to patients. In a healthcare system that is becoming increasingly vertically integrated, health plans, pharmacy benefit managers (PBMs), pharmacists and other clinical care providers and patients all have a role to play in the delivery of team-based, high-quality care. Figure 1: A Model for Vertical Integration in the Delivery of High-Quality Diabetes Care 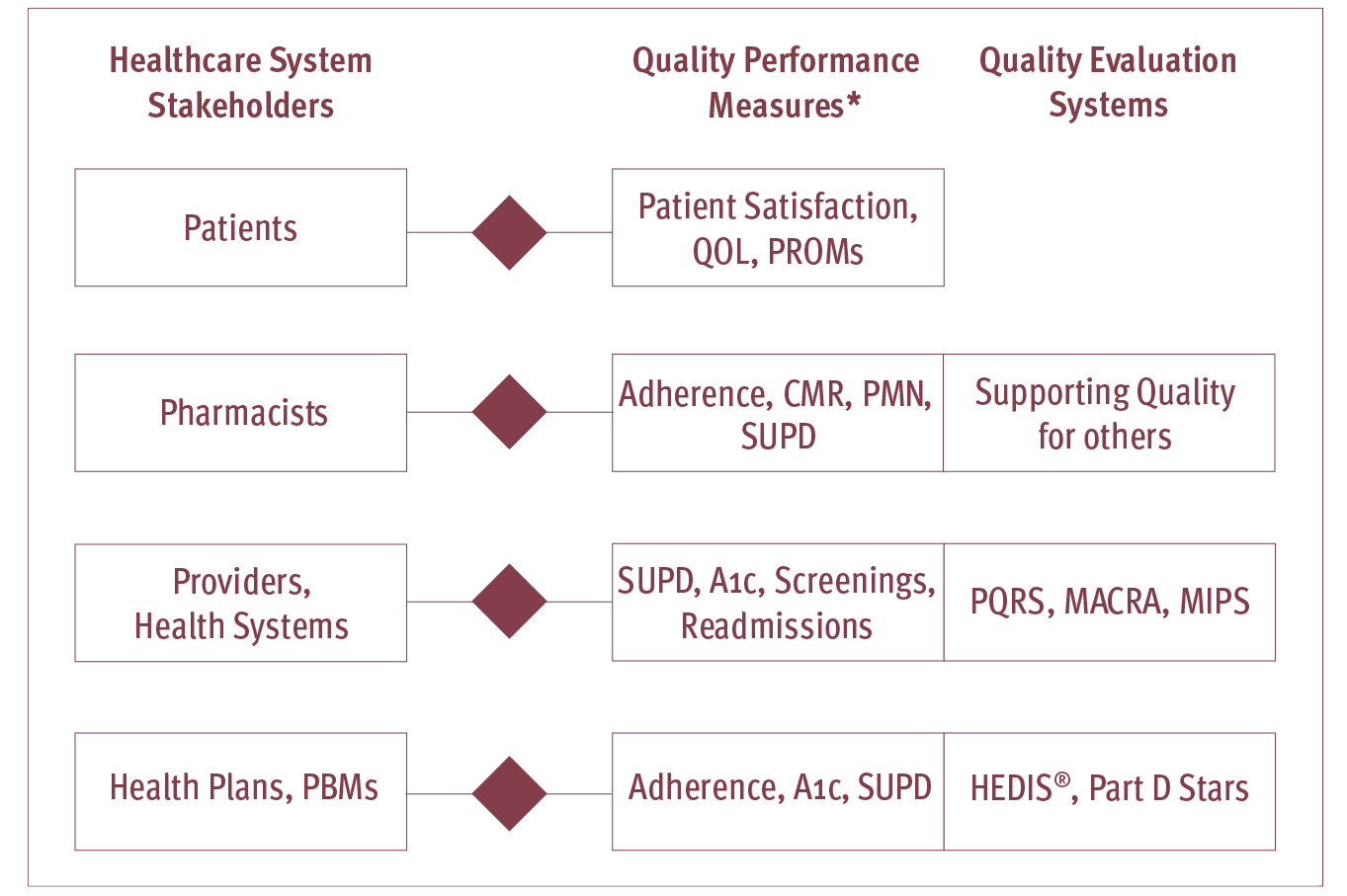
*Not limited to the listed Quality Performance Measures examples QOL: Quality of Life; PROMs: Patient Reported Outcomes Measures; Adherence: Proportion Days Covered (PDC) to oral antidiabetic medications, SUPD: Statin Use in Persons with Diabetes; CMR: Comprehensive Medication Review; PMN: Primary Medication Non-Adherence; PQRS: Physician Quality Reporting System; MACRA: Medicare Access and Chip Reauthorization Act of 2015; HEDIS®: Healthcare Effectiveness Data and Information Set; Part D Stars: Medicare Part D Star Ratings System
|
